When government agencies deem an applicant's claim for benefits, health plan coverage, or medical services insufficient, they issue denials. The appeal process allows a person to request a review of that determination. By filing properly, applicants can protect their eligibility, gain access to benefits, and resolve disputes through established procedures.
Specific provisions and laws govern denials and appeals. Agencies must issue a letter explaining the grounds for refusal, and parties generally have a set period to file an appeal. Following proper procedures is essential, as failure to comply may cause you to lose your right to benefits.
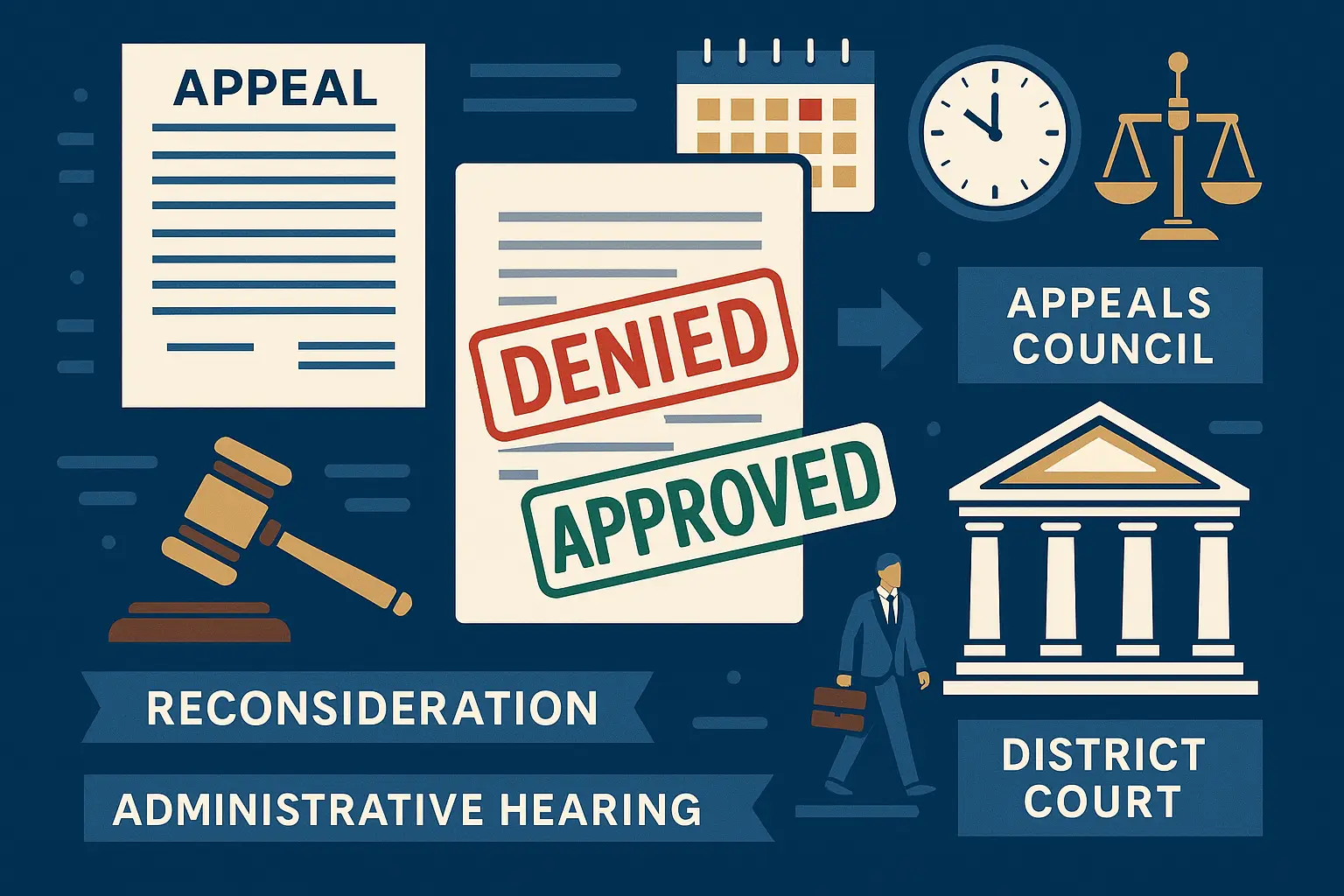
This guide explains common reasons for denial, steps for filing, required documentation, and available levels of review—from reconsideration to external review, hearings before a judge, and in some cases, petitions to the district court.
Common Reasons for Denial
Government benefit programs deny claims for many reasons. Understanding these helps applicants prepare for future filings and avoid unnecessary disputes.
- Insufficient documentation – Applications may be denied if required records, forms, or evidence are missing. Providing complete and accurate documentation is essential to verifying eligibility.
- Income or resource limits – If an applicant’s financial resources exceed the thresholds established by law, the request may be rejected. Programs must comply with specific income guidelines to ensure fairness.
- Medical criteria – Coverage may be denied if the requested treatment or condition is not included in the plan or if the medical information provided is insufficient.
- Residency or citizenship – Applicants who do not meet legal residency or citizenship requirements may be found ineligible, as program rules often mandate these criteria.
- Duplicate benefits – If an applicant already receives coverage or support for the same service, the request may be denied to prevent duplication of benefits.
- Application errors – Mistakes such as incorrect dates, incomplete information, or unsigned forms can result in a denial. Careful review before submission helps avoid these issues.
A denial letter should always note the specific reasons and provide further information about how to request an appeal.
Eligibility for Filing an Appeal
Any person denied benefits or coverage is generally entitled to file an appeal. Eligibility may extend to:
- Primary applicants denied benefits – Individuals who apply directly for benefits but receive a denial have the right to pursue further action, such as an appeal or review.
- Authorized family members or representatives – Family members or officially designated representatives may act on behalf of the applicant to submit appeals, provide documentation, or manage communications.
- Beneficiaries with reduced or terminated benefits – Individuals whose current benefits are reduced, suspended, or terminated may also challenge the decision to ensure their continued eligibility is adequately considered.
- Estate representatives – In cases involving deceased individuals, estate representatives may handle claims or appeals related to benefits on behalf of the applicant’s estate.
Applicants must file within the applicable period stated in the denial letter. Exceptions may be granted for good cause, such as illness or failure to receive proper notice. Agencies may extend deadlines, but requests must be documented and comply with existing provisions.
Step-by-Step Appeal Process
Step 1: Reconsideration
File a request for reconsideration in writing. Provide additional documentation, such as medical records, financial forms, or other evidence. A different reviewer will reconsider your claim to determine if benefits should be granted.
Step 2: Administrative Hearing
If the reconsideration is denied, request a formal proceeding before a judge. Both parties present evidence, witnesses, and records. The judge issues a written decision based on applicable laws and documentation provided.
Step 3: Appeals Council or External Review
Applicants may qualify for external review by an independent party for health plan claims. An appeals council may review the decision for other government benefits and determine if procedures were followed correctly.
Step 4: District Court Petition
If you disagree with the administrative determination, you may file a petition in district court. Courts review evidence, arguments, and legal grounds for appeal. This step may involve higher costs but provides another opportunity to resolve disputes and secure benefits.
Required Documentation for Appeals
Successful appeals depend on presenting sufficient records and evidence. Common documents include:
- Medical Documentation – Treatment notes, hospital records, prescription lists, or coverage determinations from a health plan
- Financial Documentation – Tax returns, pay stubs, and bank records showing income and expenses
- Legal Documentation – Birth certificates, marriage records, immigration forms, or military service documents
- Program Forms – Completed reconsideration forms, petitions, and appeal requests submitted by mail or online
Failure to provide required documents is a common reason appeals are denied. Applicants should review applicable requirements carefully before submitting.
Hearing and Review Process
During an appeal hearing, applicants are allowed to present their case. A proceeding before a judge is formal but provides an opportunity to resolve disputes.
- Before the Hearing – Organize documents, prepare testimony, and request additional time if necessary.
- During the Hearing – Present evidence, question witnesses, and respond to arguments from the department or insurer.
- After the Hearing – Receive a written letter noting the decision and grounds. If you disagree, you may review further or appeal to the district court.
Hearings are not public, and only parties directly involved, authorized representatives, and essential staff are permitted to attend.
Deadlines and Timelines
Appeal deadlines are strict, and missing them may result in losing the right to appeal. Applicants should carefully review the specific rules that apply to their case:
- Social Security Appeals – Applicants generally have 60 days from the date of denial to file an appeal. This applies to Social Security Disability Insurance (SSDI) and Supplemental Security Income (SSI) cases.
- Medicare Appeals – For an initial redetermination, applicants typically have 120 days from the denial date to file. Later stages of the appeal process may have shorter timeframes.
- VA Appeals – Veterans usually have up to 1 year from the date of the decision notice to file an appeal. The exact timeframe may vary depending on the chosen appeal lane (e.g., Supplemental Claim, Higher-Level Review, or Board Appeal).
- SNAP or Medicaid Appeals – Appeals must generally be filed within 90 to 120 days from the date of denial, though deadlines vary by state. It is essential to check state-specific requirements.
- Unemployment Appeals – Appeal periods for unemployment benefits are much shorter, typically 10 to 30 days, depending on state provisions. Applicants should confirm their state’s exact timeline.
Applicants should always review their denial letter for the exact deadline and submit forms promptly to avoid losing their right to appeal.
Best Practices for Successful Appeals
- Review your denial notice carefully to identify common reasons for denial.
- Gather sufficient documentation and present new evidence when possible.
- Request additional time only if you can show reasonable cause.
- File every form on time, by mail or online, following agency instructions.
- Seek authorized support from attorneys, advocates, or representatives familiar with the process.
- Prepare for hearings by organizing documents and practicing testimony.